Two subjects frequently come up in discussions of bowel care and bowel programs. The first is to talk about bowel movements. Describing stool is something that is so non-social that people have a hard time bringing it up, even to the healthcare professional. A separate issue that people struggle with is a colostomy. These are separate discussions, but both can be challenging.
Bowel Movements
People do not want to discuss their bowel movements or describe them because it is not a socially acceptable topic. However, people want to know what is "normal." The answer is normal is unique to you.
How much stool should be produced? This changes after spinal cord injury and sometimes after a head injury or with other neurological diseases. The amount of stool produced varies by your diet, the amount you move your body, fluid intake, how you feel, and the list goes on. With neurogenic bowel, messages are not well communicated to and from the brain, so the bowel slows in functioning.
The medication also affects the bowel. Those who use fiber will find their bowel movement to be huge in size compared to previous bowel activity. Those who have fluid restraints, as with intermittent catheterization, have smaller fecal output. So, the answer varies. You need to learn what is your usual amount. The important key to the size of bowel movement is that you are emptying your bowel regularly in a sufficient manner.
Do I need to have a bowel movement every day? There was a time when this was what people thought. They worked to accomplish this goal. Then people changed their thinking to just having a bowel movement when it is needed. However, the neurogenic bowel needs to be controlled for evacuation and continency. Typically, every other day is the plan. If there is breakthrough incontinence, you might choose a daily bowel program to avoid accidents. Rarely, very rarely, individuals will opt for every third day. This is not usual practice because the stool is contained in the bowel for too long, which dries it out, leading to constipation or impaction.
Everyone has a different description of their stool. Indeed, if you have neurogenic bowel, you need to look at it. People with sensation will know if they have loose stools or constipation, but you have to do a visual inspection without sensation. Based on the stool consistency, you can see if you need to adjust your diet, fluids or activity. Every bowel movement is somewhat different, so radical changes do not need to be made until you see a pattern of too loose or too dry stool.
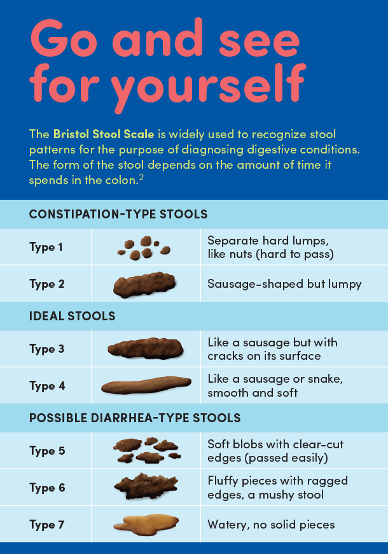
People have different opinions about stool consistency. Because everyone's description is unique, a scale was developed by the healthcare professionals in Bristol, England, aptly called the Bristol Scale. This provides consistent language about stool. It helps to identify constipation instead of just drier stool or diarrhea instead of loose stool. An accurate description helps your healthcare team understand your needs as well as not overdoing bowel treatments that slide people up and down the scale too quickly. All too often, as healthcare professionals, we see people take medication to curb diarrhea, then add medication because their stool is too dry and on it goes. The Bristol Scale puts everyone on the same page.
Here is the Bristol Scale Chart:
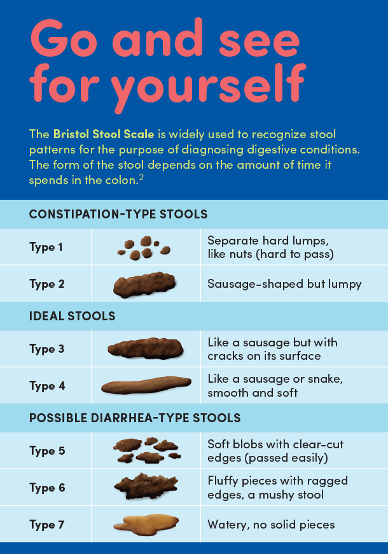
Notice that you are aiming for type 3 or type 4 stool. You can see pictured are stools with too much fluid and those with too little. But, again, look for a pattern as you adjust your bowel output consistency.
Much like everything these days, there is an app for that! There is an app for the Bristol Scale. You can download the app to monitor your stool consistency. This is an excellent tool to share with your healthcare provider for treatment decisions. Your caregiver can also follow along. If you have multiple healthcare providers and caregivers, they can see your patterns. Just remember, this is your body, so you need to know your patterns as well. Here are just a couple of sites about the apps. There are many options. You can get one from your game store. I recommend using one that is without charge. https://bristolstoolchart.net/
https://careclinic.io/stool-tracker/
https://apps.apple.com/us/app/stool-log-lite/id782394941
Colostomy
Taking a big change in gears, let's talk about a colostomy. People have a variety of opinions about the process. In healthcare, we like to keep the body functioning in its typical process. This means creating a bladder program and a bowel program. Both naturally harness body functioning to accomplish the goals of waste elimination from the body. The colostomy is considered a radical surgery and treatment plan.
A colostomy is a surgically created artificial opening in the abdomen where the bowel's large intestine is then connected. The stool is excreted through the opening. A bag is taped to the skin around the opening to collect the stool.
People have strong opinions about colostomy vs. no colostomy. This is not a time to get blinded by the thought that all problems go away with a colostomy. You must back a decision based on facts and what would be the best plan for you. If you are considering this option, think about the following issues.
With a colostomy, some people report increased quality of life because they spend less time doing a bowel program. That is enticing. Others report just a switch in bowel care activities such as instead of a bowel program, irrigation of the colostomy might be done. The bag can leak or burst at unplanned times, securing the bag is more of a challenge on a non-muscular abdomen. There can be an odor, often a person's diet has to be changed.
Skin issues can be healed or less irritated because there is less bowel incontinence to open wounds if that is an issue. However, with a colostomy, there still can be mucus passed from the rectum.
Where an elective colostomy is placed is selected by the individual with input from their healthcare professionals. This is unlike colostomy's that are done as the result of a medical condition such as bowel cancer. In medical cases, the colostomy must be placed where the medical concern can be treated. In an elective colostomy, you have some choice. Placement of the colostomy is in the ascending and transverse colon results in stools that are more liquid. In the descending colon, stools are more formed.
Quality of life is reported by most to be good with a colostomy. However, colostomy does not resolve all bowel issues, especially constipation.