Avoiding Bowel Complications-Part I
Join Our Movement
What started as an idea has become a national movement. With your support, we can influence policy and inspire lasting change.
Become an Advocate
Stool consistency
Stool should be a solid, firm consistency. Not too moist and not too dry. The unusual thing about hard or soft stool is that either way, adding fiber helps bulk up stool and makes for easier passing within the bowel. Stool can be softened using stool softener medication.
Hard stools are difficult to pass. They can over stretch the bowel as well as become so hard that an impaction develops. An impaction is stool that is blocking the bowel. Typically, no stool will pass but sometimes, liquid stool will pass around the impaction which can be confused with diarrhea. An examination can determine if there is an impaction in the lower bowel, but an x-ray is needed to establish if an impaction is higher in the bowel. Manual removal is the method for lower bowel impaction removal. Impactions higher in the bowel might require an enema or oral laxatives.
Vomiting can be the result of indigestion or illness. But it can also be due to an impacted bowel. If stool cannot move downward, it will back up through the digestive tract. Vomiting might be an indication of an impaction. You will need to look at vomit to see if there are any flakes of brown if you suspect an impaction. The flakes or flecks in vomit can be the first sign of the bowel working in reverse. Later, the flakes will be more abundant. Your vomit or breath may smell like stool.
Diarrhea is liquid stool. It occurs when the chyme moves too quickly through the bowel without time for the water and nutrients to be removed. This can occur for a variety of reasons. Illness is the primary cause. Plus, gastric distress, stress and anxiety can create an environment in your bowel for diarrhea. If you develop diarrhea, you will need to eat bland foods so as not to aggravate the bowel further. An example of a bland diet is the BRAT diet which stand for Bananas, Rice, Apple sauce and Toast. Drink electrolyte balanced fluids. Diarrhea can dehydrate you quickly. You may even need medical attention.
Bowel nerve function
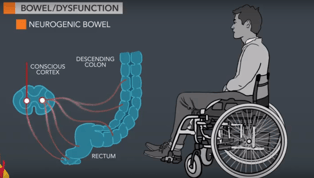
Individuals with spinal cord injury have difficulty with their bowels because of a slowing of the bowel function by the nerves of the Autonomic Nervous System (ANS) called neurogenic bowel. This nerve system slowing combined with decreased body movement affects bowel function. There is a redundant nerve system within the bowel that is also controlled by the ANS.
Many people think that because the bowels are slow, the problem is constipation. This is not the source of the problem. Treatment for constipation will not assist a neurogenic bowel to work more efficiently. A bowel program will result in controlled bowel movements with a neurogenic bowel. Individuals with or without a spinal cord injury can become constipated. You can have a neurogenic bowel and constipation. Fiber can help with both.
Bowel Program
To work well, the bowel program must be extremely regimented. You will need to reserve a time that is convenient within your lifestyle as well as consistent. For a bowel program to truly work, the time must remain the same. The bowel program is generally performed every other day. A few individuals will require an everyday program to maintain continence. The timing of the bowel program must be consistent as you are ‘training’ the bowel to work at a specific time. Consistency in timing is key.
Fortunately, the bowel is rather easy to manipulate if you are consistent. You can choose morning, evening or anytime if you keep to your selected schedule. You will get the fastest and best results by taking advantage of the gastrocolic reflex which is a stimulation of the bowel to rev up when eating. The gastrocolic reflex is strongest in the am, after breakfast. The bowel is always working, but it rests more at night so the gastrocolic reflex is strongest in the am. Doing the bowel program after the evening meal is acceptable as well. Some will take advantage of this reflex after lunch.
For individuals with Upper Motor Neuron (UMN) injury or injury in the cervical and thoracic spinal cord, a suppository is used followed by digital stimulation. Use a generous amount of lubricant so as not to injure the delicate rectal tissue. Insert the suppository gently. Use your finger to ensure the suppository is against the wall of the rectum. Perform digital stimulation gently. The goal of dig stim is to relax the internal sphincter which is about a finger’s length up in the rectum. Using too quick of a motion will not relax the internal sphincter and can cause a spasm, further tightening it and prolonging the bowel program.
Individuals with a Lower Motor Neuron (LMN) injury typically in the lumbar or sacral spinal cord have a flaccid bowel. Manual removal of stool is necessary. Still, use adequate lubricant to prevent injury to the bowel. Gently, remove the stool.
When cleaning after a bowel movement, use soap and water or toilet tissue to remove any residue that you may or may not see around the rectal area. Dry carefully and thoroughly to maintain your skin integrity.
More information about complications will be in next week’s blog. Take some time this week to review your typical bowel routine to see if you are following the best technique and program. Nurse Linda
Pediatric Consideration:
Parents or care providers will perform the bowel program for children until about school age. The child can start earlier at potty training time if you feel they have the developmental ability to do so. Have the child join in the process with you in gradual steps. Making the bowel program a natural and normal part of life helps the child to realize this process is normal for them.
The older child might not want to participate in their bowel program. Again, it will be up to the parent or caregiver to instill a sense of normalcy about the process. Most will want to complete the bowel program as quickly as possible but taking time can actually result in less time spent in the overall bowel program process.