Many individuals and reduced regulations would make you believe COVID-19 is almost over, but this would be a false assumption. Viral loads in communities go up and down with new variants. The COVID-19 virus is still among us. The COVID-19 virus will still be in the environment and will continue to be there. There are vaccinations and treatments now which help recovery. However, these are not all available to children. Therefore, precautions still need to be in place for especially vulnerable individuals, including children, those who are immunocompromised (those with limited ability to fight infections and viruses) or both.
Children who are not eligible for vaccination and who have neurological issues such as paralysis from trauma or disease are at a higher risk for COVID-19 as well as other types of infections from bacteria, viruses, fungi, and parasites. This is because the autonomic nervous system (ANS), the part of the nervous system that automatically controls immune response, can be affected. How significantly the autonomic nervous system is affected is generally unknown. The ANS can be slow to recognize an invader in the body, slow to respond to the invader, or mount no immune response at all.
In the case of COVID-19, a child with neurological issues may have minimal symptoms or a full-blown COVID infection. There is a noticeable difference in the numbers of children who have less incidence of COVID-19 development than adults. This phenomenon is still under study, but the thought is that children have a more effective immune response, less co-morbidities, and fewer ACE-2 receptors that the COVID virus prefers to attach to for entrance into the body. However, those with neurological issues may have a less effective immune response due to issues of the ANS, may have more co-morbidities and have more exposure to ACE-2 receptors in the respiratory tract but also in the urinary and bowel systems that have exposure through catheterization and bowel programs.
 Variants of the COVID virus can react differently in children than in adults. The CDC noted in December of 2021 that five times the number of all children (regardless of neurological disease) were hospitalized with the omicron variant than with the earlier delta variant.
Variants of the COVID virus can react differently in children than in adults. The CDC noted in December of 2021 that five times the number of all children (regardless of neurological disease) were hospitalized with the omicron variant than with the earlier delta variant.
The most severe cases of COVID-19 result in Acute Flaccid Myelitis (AFM). This is a serious condition of the gray matter in the spinal cord leading to flaccid muscles and reflexes. It has been associated with appearing after enterovirus infection. Noticeable peeks of the AFM occur every other year. However, with the advent of COVID-19, a major increase in AFM was noted in children who had COVID infections. AFM is typically noted with a sudden decrease in the arm and/or leg function. These symptoms may not be noticed in a child with neurological issues, so monitoring any change is important. AFM leads to respiratory failure, body temperature changes and blood pressure instability. It is life-threatening. Prompt treatment of COVID infection is necessary for an attempt to avoid this complication.
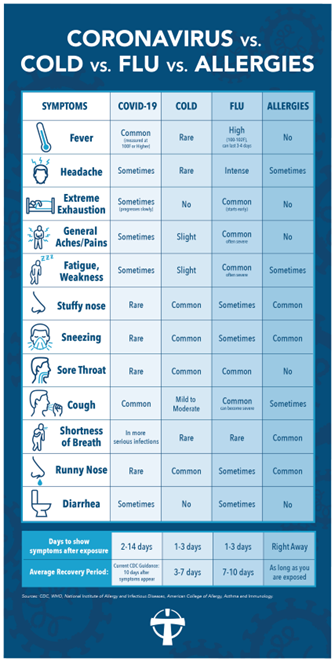
Recognizing the differences between a cold, flu, allergies, and COVID can be difficult as the symptoms are much the same. If you or your child has symptoms, it is best to get a COVID test and contact you or your child’s healthcare provider for specific instructions for treatment that is unique to you, or your child’s healthcare needs. There should be no second-guessing. Contact your child’s healthcare provider.
This chart developed by the CDC, will help you differentiate between symptoms of cold, flu, COVID or allergies. To be safe, have your child tested for COVID if you suspect it. Test yourself, and request tests for caregivers, teachers, or others in contact with your child. This chart is helpful but do not guess. Test for COVID to protect your child with neurological issues.
 Take action to prevent COVID during this time of transition. There will be many exposures to individuals who have elected not to be vaccinated or choose not to wear masks. This can place your child at an increased risk. Some preventions to take include:
Take action to prevent COVID during this time of transition. There will be many exposures to individuals who have elected not to be vaccinated or choose not to wear masks. This can place your child at an increased risk. Some preventions to take include:
Vaccine:
Get a COVID vaccination for your child if they are eligible. This includes their age as well as their unique medical condition. Discuss the benefits and risks of the vaccination for your child’s unique health situation with their healthcare provider.
Get a vaccination for everyone who is eligible in your family.
Discuss with your healthcare provider if others who care for your child should be vaccinated. This includes caregivers, teachers, healthcare providers, friends, relatives, and anyone in close contact with your child.
Vaccines are shown to slow the spread of COVID.
Masks:
Insist on mask-wearing and that the mask must be worn correctly over the nose and mouth. If your child is over the age of two and has hand function, they should wear a mask. If your child is unable to wear a mask, those caring for your child or those exposed to your child should wear a mask for your child’s protection. Otherwise, both the child and those interacting with your child should wear a mask for protection. The pandemic has demonstrated that wearing a mask is an effective deterrent in spreading COVID as well as other infections.
The most protective masks are N95, KN95, and hospital-type masks. Pick a mask that is the correct size for your child. Wearing a mask that is too large or too small will not provide effective protection.
Many individuals will insist that mask-wearing is no longer necessary, but this is not true for those who are immunocompromised. COVID is still active in the community. Your child is vulnerable. Wear your mask proudly so your child will as well.

 Variants of the COVID virus can react differently in children than in adults. The
Variants of the COVID virus can react differently in children than in adults. The 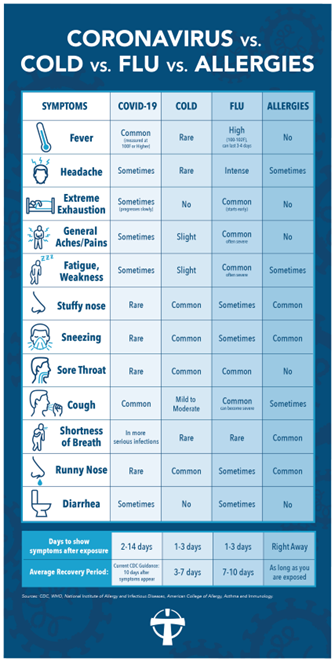 Take action to prevent COVID during this time of transition. There will be many exposures to individuals who have elected not to be vaccinated or choose not to wear masks. This can place your child at an increased risk. Some preventions to take include:
Take action to prevent COVID during this time of transition. There will be many exposures to individuals who have elected not to be vaccinated or choose not to wear masks. This can place your child at an increased risk. Some preventions to take include: