 Traumatic spinal cord injury can be associated with a head injury, especially if the SCI is to the upper spine, but anyone with an SCI can also have a head injury. Estimates of spinal cord injury and head injury vary and are not yet reliable. Some estimate as many as 30-60% of individuals with spinal cord injury have a traumatic brain injury at the same time as the original trauma. Therefore, it can be confusing why these two traumas have not been linked more closely and discussed publicly.
Traumatic spinal cord injury can be associated with a head injury, especially if the SCI is to the upper spine, but anyone with an SCI can also have a head injury. Estimates of spinal cord injury and head injury vary and are not yet reliable. Some estimate as many as 30-60% of individuals with spinal cord injury have a traumatic brain injury at the same time as the original trauma. Therefore, it can be confusing why these two traumas have not been linked more closely and discussed publicly.
Some of the reasons could be that immediately after a high-level spinal cord injury, life-threatening measures have to be instituted. The patient may be unconscious, or soon after being admitted to a hospital, heavy medications and anesthesia are administered. Rightly so, to combat the effects and provide treatment for the immediate treatment of spinal cord injury. This can make an assessment of a brain injury impossible at the time.
As the patient recovers and wakens, which may take days or, even less often, weeks, the subtle signs of a head injury may be dulled or confused with complications from wakening from anesthesia. The memory of the accident may be blurred. This is alright, as the devastation of the trauma is not something people need to recall in detail. The lasting effects speak enough.
Some head injuries are obvious if there is a wound that penetrates the skull. This is easily seen, so the diagnosis is quickly made. However, less obvious head injuries cannot be seen, even with imaging scans.
Open head injuries such as wounds, especially those that disrupt the skull, can be seen and then evaluated for potential brain injury.
Closed head injuries are those that occur inside the skull where the trauma cannot be seen by looking at the person. The anoxic head injury occurs to the whole brain and nervous system, including the spinal cord - when the oxygen supply is interrupted. Coup counter coup injury occurs when the brain bounces against the skull. Unfortunately, if there is enough force to bounce the brain against the skull, it will usually repel backward to the opposite side of the skull, creating two injuries, one to opposite sides of the brain. These can be front and back, side to side or any combination or directions.
A concussion is a closed head injury that can be very mild to very severe. Concussions can affect one area of the brain or the entire brain. Less severe concussions that affect only one small part of the brain can be difficult to diagnose because the symptoms are often not very clear. If you are feeling you are not quite grasping what the patient is saying or doing, it is probably the result of a concussion. The healthcare provider or family care provider has to be very astute to note subtle changes in the person’s behavior which may be general or even just in one particular activity. Noting changes, even subtle changes, can be very important in diagnosing and treating a head injury.
Some head injuries might not be noticed until much later as the individual recovers from the trauma of the event. It might not even be until a person returns home that the family notices, that they cannot retain information or perhaps do simple math calculations like handling money. Sometimes, the head injury results are not noted until the individual returns to the higher-level challenges of work or school. This is because of the safe and routine environment of the rehabilitation setting, where life occurs in a highly organized routine. The functional flow of the facility is built for the convenience of the patients as opposed to the reorganization and thinking that is required to make your home fit your new needs.
There are several clues to knowing if you have had a head injury in addition to a spinal cord injury. An obvious head injury will be diagnosed immediately or assessed when an individual is able to answer questions in the health care setting. A less obvious head injury might not be diagnosed as the higher-level functions of the brain may not be tested until real situations arise.
One way to think about the possibility of a head injury is to think about how your injury occurred. If you have a high-level spinal cord injury, it is reasonable to think about the ability of the very small structure of the neck being able to support the weight of your head. The neck has a lot of weight to support with little musculature. Once the head gets the force of movement during a trauma, there is little the neck can do to support the kinetic motion of the head.
There are many causes of spinal cord injuries that are prone to coincide with a traumatic head injury. Anything that obstructs the airway can lead to anoxic injury. This can include stopping breathing during the accident or a water obstruction from drowning or choking. The brain is normally floating in cerebral spinal fluid to keep it from hitting the skull in normal movement. However, the force of an injury can cause the brain to bounce against the skull leading to a bruise or bleeding in the brain. This type of acceleration injury can lead to a head injury.
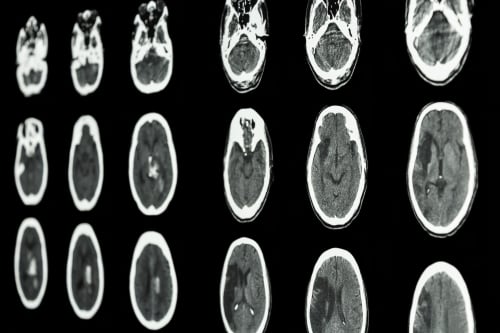
Testing for head injury can be done with CT or MRI scanning. In the ICU, monitoring of internal head pressure may be done. However, the more subtle types of a head injury may not show up in scans. Testing of mental function by a neuropsychologist or speech and language therapist may be needed to assess the functions of how the brain works. Family members or nurses at the bedside are typically the people who first pick up on ‘slight mental changes. These are important clues to see what can be done to help recovery.
Treatments for head injury are provided by your healthcare professional. Some head injuries that are mild will have a natural recovery over time. Most head injuries will require interventions for recovery that are specifically tailored to the location of the injury in the brain. Open head injuries, removal of blood clots in the brain or repair of a broken blood vessel (aneurysm) will require surgery. Closed head injuries will be treated with therapies specific to the unique needs of each individual. Some people will require quiet periods to rest their brains. Others will require puzzles and challenges. Follow the recommendations that are provided by your healthcare provider carefully. Challenging a brain that needs rest will create more problems for the individual. Too many challenges or too little can be frustrating to an individual. Practice sessions may be limited to a short amount of time.
Behavior issues can be a significant part of a head injury. This does not occur in all cases but acting out, or an inability to control behavior can occur. Changes in your family member’s temperament can be from adjustment to spinal cord injury but can also be from brain injury or a combination of both.

 Traumatic spinal cord injury can be associated with a head injury, especially if the SCI is to the upper spine, but anyone with an SCI can also have a head injury. Estimates of spinal cord injury and head injury vary and are not yet reliable. Some estimate as many as 30-60% of individuals with spinal cord injury have a traumatic brain injury at the same time as the original trauma. Therefore, it can be confusing why these two traumas have not been linked more closely and discussed publicly.
Traumatic spinal cord injury can be associated with a head injury, especially if the SCI is to the upper spine, but anyone with an SCI can also have a head injury. Estimates of spinal cord injury and head injury vary and are not yet reliable. Some estimate as many as 30-60% of individuals with spinal cord injury have a traumatic brain injury at the same time as the original trauma. Therefore, it can be confusing why these two traumas have not been linked more closely and discussed publicly.